Menopause: A Comprehensive Guide to the End of Menstruation
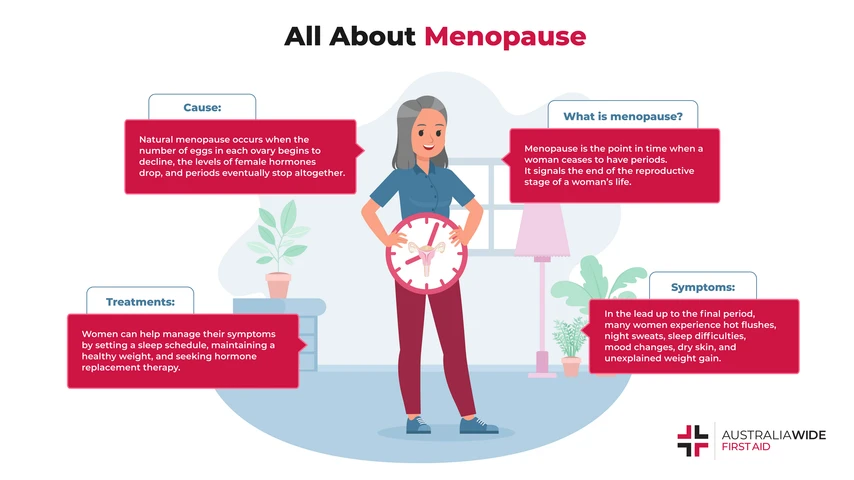
Menopause is the point in time when a woman, trans man, or non-binary person assigned female at birth ceases to menstruate (have periods).
A person is generally considered postmenopausal when they not had a period for 12 consecutive months.
Most people experience menopause naturally between the ages of 45 and 55, though some may experience menopause prematurely due to surgical interventions, medical treatments, or health conditions.
Menopause is known to cause several uncomfortable and potentially debilitating symptoms, including hot flushes, night sweats, and mood changes. Many of these symptoms can be reduced through lifestyle changes - however, if they begin interfering with your daily function, you may need to seek medical support.
Menopause is the point in time when a woman, trans man, or non-binary person assigned female at birth ceases to menstruate (have periods). It signals the end of the ability to fall pregnant. Clinically, it refers to the last or final menstrual period.
Natural menopause generally takes place when between 45 and 55 years of age, with an average age of 51 here in Australia.
There are three distinct stages of menopause - perimenopause, menopause, and postmenopausal.
Diagnosis of menopause involves identifying and tracking symptoms. Measuring hormonal changes is not a recommended way to diagnose menopause (unless premature menopause is suspected), due to the significant fluctuations that may occur naturally during this time, and as the results don't change the management approach.
There are a number of causes of menopause, including naturally, through surgery, or through medical treatments.
Naturally, menopause occurs due to a loss of ovarian follicles (a small, fluid filled sac that contains one immature egg), the follicles stop developing (follicular development) and releasing mature eggs (ovulation). At the same time, the body stops producing certain hormones regularly, including oestrogen and progesterone. In simpler terms, the supply of mature eggs drops, and ovulation becomes irregular. At the same time, hormone production decreases. Oestrogen is responsible for developing and maintaining the female reproductive system, while progesterone helps regulate menstruation and support pregnancy.
When a woman stops menstruating due to surgical interventions, this is known as surgical menopause. When a woman stops menstruating due to medical treatments, this is known as induced menopause.
Some surgeries and medical conditions can cause menopause to occur before the body would naturally:
Oophorectomy, an operation in which one or both ovaries are removed. Oophorectomies are commonly performed to remove an ovarian cyst, a twisted ovary, or if there is a risk of ovarian cancer.
Cancer treatments, including chemotherapy and radiotherapy. Chemotherapy uses powerful drugs to kill fast-growing cells in the body. The cells of the ovaries (oocytes) tend to divide quickly, and so are often impacted by chemotherapy. This can lead to infertility and early menopause, as oocytes produce hormones that help release eggs each month and prepare the uterus for possible pregnancy.
Health conditions, such as primary ovarian insufficiency (POI), when the ovaries cease functioning before the age of 40. There are many possible causes of POI, including chromosomal abnormalities, autoimmune diseases, and metabolic disorders. More often than not, however, the exact cause remains unclear.
There are three stages of menopause, including:
Perimenopause is largely considered the ‘lead-up’ to natural menopause - the time leading up to menopause to one year after menopause. It occurs when the ovaries begin running out of eggs, which causes the body’s levels of female hormones to fluctuate dramatically. As such, you may stop ovulating regularly, which can impact the frequency, intensity, and duration of your periods. The onset of perimenopause is not predictable, and can be as early as 10 years from the final menstrual period. Similarly, there is no way to predict how long perimenopause will last for you.
Perimenopause is often signalled by changes to the menstrual cycle, including irregular periods, changes in flow, and changes in the length of your cycle. These particular symptoms can be masked if you are using hormonal birth control.
Using hormonal birth control does not impact when you go through menopause, and is still necessary to prevent pregnancy during this time if that is your choice of contraception.
Aside from the changes to your actual period, perimenopause is characterised by a range of other physical, mental, and emotional symptoms.
Perimenopause generally affects women in their 40s, and on average it lasts for 4 to 6 years. Most women only experience mild to moderate symptoms during perimenopause. However, if your symptoms are so severe that they are impacting your daily life, you should consult a healthcare professional.
Menopause is the final period, and a woman is considered to have reached menopause when they have not had a period for 12 months. It occurs when the ovaries run out of eggs, and the body can no longer ovulate or have periods. As we mentioned earlier, the symptoms often associated with menopause, such as hot flushes, mood changes, and unexplained weight gain, are generally felt before a woman reaches menopause.
Postmenopause starts when a woman has not had periods for 12 months.

The symptoms often associated with menopause are generally felt more intensely during perimenopause. As these symptoms can last on average for 7 years, that means they are around for about a tenth of a person's life.
20% of women, trans men, and non-binary people assigned female at birth report experiencing no menopausal symptoms. That means that 80% will. As stated by the Australasian Menopause Society states, cessation of physiological production of oestrogen at the menopause may result in sequelae ranging or ‘raging’ from unpleasant to pathological.
These symptoms can include:
Hot flush refers to a feeling of extreme heat in the face, neck and chest, and often occurs alongside a visible flush or reddening of these areas. The body compensates for this feeling of extreme heat by sweating, sometimes profusely. This combination leads to disturbed sleep and 'night sweats'. This particular combination of symptoms is the hallmark of menopause, with up to 75% of people experiencing this. The average duration of episodes of hot flushes and night sweats is 7 years, and for 25% of people who experience them, they are classed as severe.
There is a 50% decrease in serotonin (a chemical that regulates mood, emotions and sleep) after menopause with declining oestrogen levels. Depression is not more common at menopause than at other stages of life, but a past history of depression, particularly post-natal depression, and stress during perimenopause may make a woman more likely to succumb to mood problems.
It cannot be understated how the combination of sleep disturbance with the host of other possible symptoms has an adverse affect on quality of life, mental health, relationships, careers, and wellbeing.

Treating the symptoms of perimenopause and menopause requires a comprehensive assessment including symptoms, risk of chronic disease, lifestyle and appropriate screening. An individual treatment plan should be developed with your health care team, incorporating your treatment goals alongside a risk benefit analysis.
There are several treatment options available to help women manage menopause symptoms and reduce their risk of menopause complications. These can include lifestyle changes, non-pharmacological, contraception, non-hormonal and menopausal hormone therapies.
MHT refers to the medical replacement of oestrogen, progesterone, and (sometimes) testosterone. The combination of hormones used, and their dosage, will be individually prescribed to you based on your medical history and needs.
It can provide relief from several menopausal symptoms, including hot flushes, night sweats, mood swings, insomnia, and vaginal dryness. Oestrogen therapy can also prevent bone loss, reducing the risk of osteoporosis and postmenopausal bone fractures.
MHT is the most effective treatment currently available for hot flushes and night sweats. By alleviating these symptoms, many of the secondary symptoms associated with sleep disturbances are also reduced.
As with any medical treatment, MHT is not without its risks, including blood clots, breast cancer, and stroke. However, these risks are considered small and inconsequential compared with the overall benefits of MHT. Non-oral routes of administration present fewer risks than oral preparations. MHT is not associated with weight gain.
It is important to note that evidence for the effectiveness of lifestyle and behaviour modifications for menopausal symptoms is mixed, limited or non-existent. Lifestyle and behavioural modifications might not necessarily improve symptoms, but some may improve wellbeing and help women tolerate symptoms.
Sleep
It is not uncommon to experience sleep difficulties before, during, and after menopause. Most menopausal women, trans men, and non-binary people identified as female at birth attribute their sleep difficulties to hot flushes and night sweats, as these can disturb your sleep pattern and trigger insomnia. Insomnia is a common sleep disorder in which a person struggles to fall and stay asleep. You can improve your sleep quality by taking a close look at your sleep habits. You may nee to establish or alter you regular sleep schedule, comfortable sleeping environment, pre-bedtime routine, and fostering good sleeping habits during the day, such as exercising and getting a good dose of daylight. More tips for getting a good night's sleep can be found in our Article Library.
Weight and Exercise
Weight gain during menopause may increase the severity of some symptoms such as hot flushes and night sweats. Maintaining a healthy weight for your body may help to alleviate these symptoms. Exercise hasn't been shown to have any impact on hot sweats or night sweats. It may, however, have impacts on other aspects of health and wellbeing and on quality of life.
Environment
As hot flushed and night sweats are the most common symptom, it may be worthwhile to adjust your environment where possible. This could include adjusting clothing, using a hand fan or electric fan as required, keeping your bedroom and bedding cool at night, and drinking cool liquids.
Avoiding triggers
Some people may be able to identify triggers for hot flushes and night sweats, such as spicy foods, smoking, or alcohol. If you can identify a trigger, you may be able avoid these or adapt your approach.
Cognitive Behaviour Therapy
Group and individual cognitive behaviour therapy are both effective at reducing the impact of some symptoms such as hot flushes, and at improving sleep and general wellbeing. These could be used in conjunction with other therapies or treatments.
Other
Other techniques have varied rates of efficacy for lessening the impact of symptoms. These include yoga, paced breathing, relaxation, hypnosis, acupuncture. It is worth noting that magnetic therapy, reflexology, and chiropractic interventions have no evidence of benefit. There is currently insufficient evidence to support the use of herbal therapies to treat menopausal symptoms, and they may not be safe in some women.
After menopause, a woman’s risk of certain medical conditions increases, including:
Cardiovascular disease (CVD):
CVD refers to any condition affecting the heart and blood vessels. It is often caused by atherosclerosis, a condition in which fats, cholesterol, and other substances build up in the inner lining of arteries to form plaque. This build-up of plaque can reduce the heart’s blood flow temporarily, as in angina (chest discomfort), or it can block the heart’s blood flow completely, as in a heart attack. Heart attacks can be fatal, as the longer the heart goes without oxygen, the greater the chance it will sustain permanent damage and begin to fail. Menopause can drive certain risk factors for CVD. According to the Australasian Menopause Society, a drop in oestrogen levels can increase the level of fat in a woman’s blood. This can subsequently result in high cholesterol and blood pressure, both of which can weaken blood vessels and make them more prone to clotting.
Osteoporosis:
Osteoporosis means ‘porous bones’. It is a condition in which bones become thin, weak, and prone to fractures. Bone is a living tissue that comprises various cells, proteins, and minerals. They are in a constant state of renewal, with old bones being broken down to make way for new ones. Osteoporosis occurs when old bone tissue is lost faster than the body can replace it. There are numerous risk factors for osteoporosis, including low body weight, calcium intake, and vitamin D levels. Menopause can also trigger certain risk factors for osteoporosis, as oestrogen regulates the activity of osteoblasts, cells that make new bone. As such, low oestrogen levels can decrease a woman’s bone mineral density and make them more susceptible to osteoporosis.
Urinary Incontinence:
Urinary incontinence is when urine leaks from the urethra involuntarily. It can occur when the bladder muscles suddenly tighten, such as when a person coughs, sneezes, or laughs, but the sphincter muscles are not strong enough to pinch the urethra shut. There are various types of urinary incontinence, all of which can result from a host of different lifestyle habits, medical conditions, or physical problems, such as pregnancy, alcohol consumption, and urinary tract infections. Menopause can also increase a woman’s risk of urinary incontinence. This is because oestrogen plays a key role in maintaining the elasticity of vaginal tissue, the thickness of the urethra, and the strength of the pelvic floor (the muscles that support the urethra and bladder). As such, low oestrogen levels can increase the frequency and urgency of a woman’s need to urinate.
Now that women live around one third of their lives after menopause, optimising physical and mental health during this period is becoming more important.

Menopause is the point in time when a woman, trans man, or non-binary person assigned female at birth ceases to have periods. It occurs naturally when the ovaries run out of eggs and the body can no longer ovulate.
Menopause comes in three stages: perimenopause, menopause, and post menopause. It is during perimenopause, when ovaries begin running out of eggs, that woman, trans man, or non-binary person assigned female at birth typically experience the symptoms closely associated with menopause.
These symptoms can include hot flushes, night sweats, and mood changes. Menopause can also trigger susceptibility to certain health conditions, including cardiovascular disease, osteoporosis, and urinary incontinence.
There are several treatment options available to you, and these should be discussed with your health care team. If you are concerned, seek out a specialist in women's health specifically.
Menopause is a natural part of life, and no woman, trans man, or non-binary person assigned female at birth should feel ashamed for going through the ‘change of life’. There are plenty of resources and information available to help you navigate any uncertainty.

March 25, 2025
Explore non-traditional paths to sobriety, including mindfulness, yoga, nutritional therapy, and community-based support, for a personalized approach to recovery.
September 7, 2022
Menopause is the final period, when a woman, trans man, or non-binary person assigned female at birth's ovaries run out of eggs and the body can no longer ovulate. Menopause comes with several symptoms, complications, and treatment options.
July 26, 2024
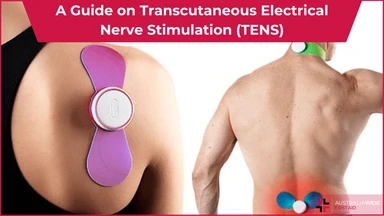
Transcutaneous Electrical Nerve Stimulation (TENS) is a therapeutic method of pain relief. It utilises an electrical device that emits electrical currents and streams the impulses via electrode patches attached to the skin.